Infertility and Reproductive Health: Understanding the Challenges and Solutions
Infertility affects millions of people worldwide and can be a source of profound emotional, physical, and social hardship. It is a complex condition influenced by various factors, including genetics, lifestyle, environmental influences, and underlying health conditions. This comprehensive guide explores the causes of infertility, its impact on reproductive health, and various treatments and lifestyle modifications that can help couples achieve pregnancy.
1. Understanding Infertility
Infertility is defined as the inability to conceive a child after one year of regular, unprotected intercourse for women under 35, or after six months for women over 35. It affects both men and women and can stem from multiple causes related to reproductive anatomy, physiology, or hormonal imbalances.
Types of Infertility:
- Primary Infertility: When a couple has never been able to conceive.
- Secondary Infertility: When a couple has previously conceived but is now unable to achieve pregnancy.
Example: A couple who had a successful pregnancy five years ago may face difficulties conceiving again, which would be categorized as secondary infertility.
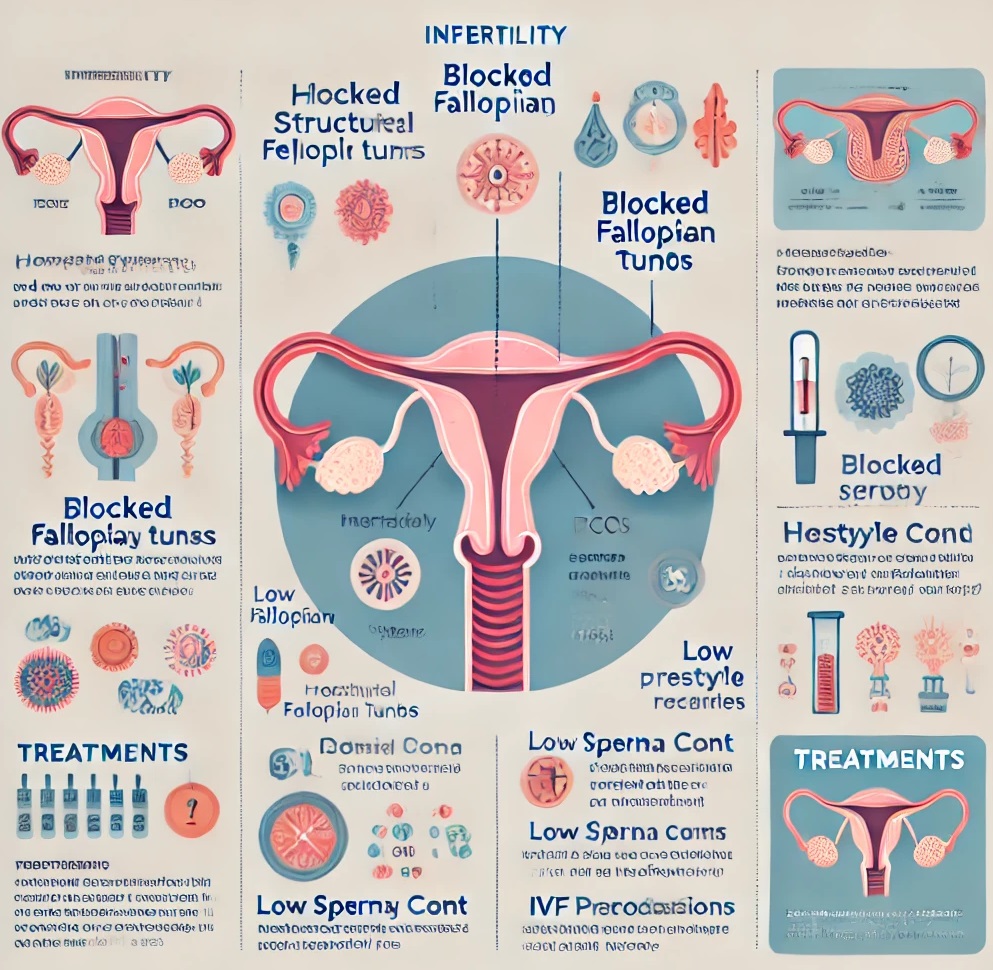
2. Causes of Infertility in Women
Several factors can contribute to infertility in women, including ovulatory disorders, structural problems, and hormonal imbalances.
a) Ovulatory Disorders
- Polycystic Ovary Syndrome (PCOS): One of the most common causes, affecting ovulation due to hormonal imbalances.
- Thyroid Disorders: Both hyperthyroidism and hypothyroidism can disrupt menstrual cycles.
- Premature Ovarian Insufficiency: Occurs when the ovaries stop functioning before age 40, reducing fertility potential.
Example: A woman with PCOS may experience irregular periods or lack of ovulation, making it challenging to conceive naturally.
b) Structural Problems
- Blocked Fallopian Tubes: Often caused by infections like pelvic inflammatory disease (PID) or endometriosis, blocked tubes can prevent the sperm from reaching the egg.
- Uterine Fibroids: Benign growths in the uterus can interfere with embryo implantation.
Example: A woman with a history of PID may develop scarring in her fallopian tubes, hindering fertilization.
c) Hormonal Imbalances
- Hyperprolactinemia: Excess production of prolactin can interfere with ovulation.
- Low Progesterone Levels: This hormone is crucial for maintaining early pregnancy. Low levels may lead to implantation failure.
3. Causes of Infertility in Men
Male infertility is often due to issues with sperm production, delivery, or quality. Factors contributing to male infertility include genetic conditions, lifestyle, and environmental exposure.
a) Sperm Disorders
- Low Sperm Count: A count of fewer than 15 million sperm per milliliter of semen is considered low.
- Poor Sperm Motility: If sperm cannot swim properly, they may not reach or fertilize the egg.
- Abnormal Sperm Morphology: Poorly shaped sperm may struggle to fertilize an egg.
Example: A man with low sperm count and motility issues may have difficulty impregnating his partner.
b) Hormonal Causes
- Hypogonadism: Reduced hormone production by the testes can result in low sperm count.
- Elevated Estrogen Levels: Excess estrogen can suppress testosterone production, impacting sperm quality.
c) Structural Problems
- Varicocele: An enlargement of the veins within the scrotum can reduce sperm quality.
- Obstructions: Blockages in the ducts that transport sperm may prevent it from mixing with semen.
4. Diagnosing Infertility
Infertility diagnosis often involves a series of tests and assessments for both partners. Some common diagnostic tests include:
- Hormonal Testing: Blood tests to measure hormone levels, including estrogen, progesterone, testosterone, and FSH (follicle-stimulating hormone).
- Ultrasound Imaging: Helps identify structural problems such as uterine fibroids or ovarian cysts.
- Semen Analysis: Evaluates sperm count, motility, and morphology.
- Hysterosalpingography (HSG): An X-ray that checks for blockages in the fallopian tubes.
5. Impact of Lifestyle and Environmental Factors
Lifestyle and environmental factors play a significant role in fertility. Unhealthy habits and exposure to toxins can negatively impact reproductive health in both men and women.
a) Lifestyle Factors
- Diet: A balanced diet rich in nutrients supports reproductive health. Deficiencies in vitamins, such as Vitamin D and folic acid, may impair fertility.
- Exercise: While moderate exercise promotes health, excessive physical activity can lead to hormonal imbalances and menstrual irregularities.
- Weight: Being underweight or overweight can disrupt menstrual cycles in women and reduce sperm quality in men.
b) Environmental Factors
- Exposure to Toxins: Chemicals such as pesticides, heavy metals, and endocrine disruptors can interfere with hormonal balance.
- Smoking and Alcohol: Both can reduce sperm quality and increase the risk of miscarriages.
6. Treatment Options for Infertility
Treatment for infertility depends on its cause, ranging from medication and lifestyle adjustments to advanced reproductive technologies (ART).
a) Medications
- Clomiphene Citrate: Often prescribed to women with ovulation issues, stimulating egg production.
- Gonadotropins: Hormone injections that stimulate multiple egg releases.
- Metformin: Used in cases of PCOS to improve insulin sensitivity and support ovulation.
b) Assisted Reproductive Technology (ART)
- Intrauterine Insemination (IUI): Sperm is inserted directly into the uterus around ovulation to increase the chances of fertilization.
- In Vitro Fertilization (IVF): Involves fertilizing an egg outside the body and implanting the embryo into the uterus.
- Intracytoplasmic Sperm Injection (ICSI): A single sperm is injected directly into an egg, often used in cases of male infertility.
Example of IVF Process:
- Ovarian stimulation to produce multiple eggs.
- Retrieval of mature eggs from the ovaries.
- Fertilization of eggs with sperm in a lab.
- Implantation of embryos into the uterus.
c) Lifestyle Modifications
- Diet and Exercise: Adopting a balanced diet and regular physical activity can improve fertility.
- Reducing Stress: High stress levels can disrupt hormonal balance and impact reproductive health.
- Avoiding Toxins: Minimizing exposure to chemicals in personal care products and the environment can improve reproductive outcomes.
7. Psychological and Social Impact of Infertility
Infertility can significantly impact mental health and social relationships. The emotional toll of infertility treatments, coupled with societal pressures, can lead to stress, anxiety, and depression.
a) Coping Mechanisms
- Counseling and Support Groups: Many people find comfort and support in counseling sessions or fertility support groups.
- Mindfulness and Stress Management: Techniques like meditation and yoga can help manage the emotional aspects of infertility.
8. Case Study: A Couple’s Journey Through Infertility
Scenario: Sarah and John have been trying to conceive for over two years. Sarah is diagnosed with PCOS, and John has a lower-than-normal sperm count. After discussing options with a fertility specialist, they decide to try IVF. Following hormone treatments and egg retrieval, several eggs are fertilized and a viable embryo is implanted in Sarah’s uterus. After a difficult journey, Sarah becomes pregnant, and the couple achieves their dream of parenthood.
9. Preventive Measures and Health Maintenance
While not all infertility cases are preventable, maintaining reproductive health can improve fertility prospects.
a) Regular Check-Ups
- Screening for STIs: Many sexually transmitted infections, if left untreated, can lead to scarring and blockages.
- Monitoring Menstrual Health: Keeping track of menstrual cycles can help identify potential ovulatory issues early.
b) Education and Awareness
- Family Planning and Safe Practices: Understanding fertility windows and using contraceptives wisely can prevent unintended impacts on reproductive health.
- Avoiding High-Risk Behaviors: Reducing risky behaviors, such as smoking and heavy alcohol consumption, helps protect fertility.